
Dirk Stanley, MD, CMIO, UConn Health
How do you say ‘Lumbar Puncture’ in CPOE? Today, I’m writing to share the translation of one of the oldest, most common medical procedures that’s routinely done in modern healthcare: The lumbar puncture, sometimes referred to as an ‘LP.’
This procedure is done to help look for infections, malignancy, and antibodies and other markers of neurologic disease. While they are a common mainstay of modern healthcare, building LPs electronically can be quite a challenge.
Want to reduce clicks when ordering your LPs? It helps to first have a solid understanding of the most common LP workflows in healthcare, so you can build your order sets with the most common studies, priorities, indications, and order statuses all properly built and correctly defaulted.
So in this post, I figured I’d share some secrets about the four most common lumbar puncture workflows, and how to build them into an EMR in a really gourmet fashion to ensure the best diagnostic yield, fewest clicks, and maximal success.
- The Workflows
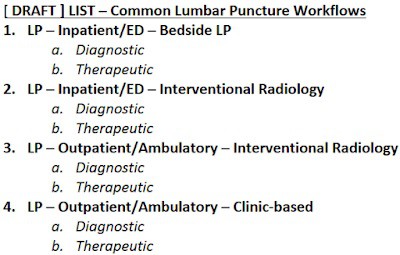
Lumbar punctures are commonly done for diagnostic purposes, but can also sometimes be done for therapeutic purposes. But as it turns out, the LP is not just one workflow; it’s actually four different workflows.
In each of these scenarios, there are different clinical specialties using the LP commonly for different purposes.
In addition to these workflow descriptions, some helpful notes:
- In workflows #2 and #3 above, there is often a communication challenge between the ordering provider and the Interventional Radiologist, who has to collect, label, and transport the samples to the lab, as well as report some findings back to the ordering provider (e.g. opening pressures, turbidity, etc.).
- In workflow #3 above, there is also sometimes a patient education challenge, whereby the patient needs to come before the scheduled interventional radiology LP to have ‘pre-procedure’ labs drawn (e.g. CBC, BMP, PT/INR) to help ensure that the LP can proceed without problems.
- The Stakeholders
Given the above workflows, the physician specialties most commonly involved with lumbar punctures then include:
- Emergency Medicine
- Inpatient Physicians – Pulmonary/Critical Care (Intensivists)
- Inpatient Physicians – General Inpatient Medicine (Hospitalists)
- Interventional Radiologists (IR)
- Ambulatory/Inpatient Specialists – Infectious Disease Physicians
- Ambulatory/Inpatient Specialists – Neurologists (General)
- Ambulatory/Inpatient Specialists – Neurologists (Movement Disorders)
- Ambulatory/Inpatient Specialists – Neurologists (Multiple Sclerosis)
- Ambulatory/Inpatient Specialists – Neuro-ophthalmologists
- Ambulatory/Inpatient Specialists – Hematology/Oncologists
If we include the following:
- Registered Nurses (who have to help care for the patient before/after lumbar punctures),
- Pharmacists (who help provide the medications the provider has ordered for sedation/anesthesia)
- Laboratory workers (who receive the fluid, provide the on-site analysis of certain labs, and send out other labs to external labs)
- IT/Informatics workers (who connect with stakeholders, map the current state, and work with the clinical stakeholders to design, build, and test the future state)
Then this gives us a fairly long list of stakeholders in the most common lumbar puncture workflow discussions:
- Emergency Medicine Providers
- Inpatient Physicians – Pulmonary/Critical Care (Intensivists)
- Inpatient Physicians – General Inpatient Medicine (Hospitalists)
- Interventional Radiologists (IR)
- Ambulatory/Inpatient Specialists – Infectious Disease Physicians
- Ambulatory/Inpatient Specialists – Neurologists (General)
- Ambulatory/Inpatient Specialists – Neurologists (Movement Disorders)
- Ambulatory/Inpatient Specialists – Neurologists (Multiple Sclerosis)
- Ambulatory/Inpatient Specialists – Neuro-ophthalmologists
- Ambulatory/Inpatient Specialists – Hematology/Oncologists
- Nursing – Interventional Radiology
- Nursing – Floor/Bedside
- Nursing – Clinics
- Laboratory
- Pharmacy
- Clinical IT/Informatics
You’ll quickly see why it’s helpful to have a good clinical informatics and project management team available to help coordinate all of the meetings, discussion, architecture, building, testing, and approvals before you can go-live. In short, optimizing LP order sets is usually a significant project effort, requiring many meetings.
- The Labs
With regard to the actual laboratories, it’s helpful to keep in mind that workflows #1 and #2 are general-purpose LPs, usually for the emergent ruling out of CNS infection. It typically doesn’t get much more complicated than that. So for Inpatient/ED purposes, the most common studies include:
- CSF Cell Count and Differential
- CSF Gram Stain and Culture
- CSF Protein
- CSF Glucose
- Occasionally CSF HSV PCR, if clinically indicated
Workflows #3 and #4, however, are more specialty-oriented, and so their labs may include the general labs above, as well as a number of complex, high-cost specialty panels, antibodies, proteins, and pathology/flow cytometry.
Commonly, the occasional ordering of these specialty studies (commonly from workflows #3 and #4 above) in the Inpatient/ED settings (commonly workflows #1 and #2 above) can generate a lot of discussion. For reimbursement reasons, it’s helpful to stratify these workflows, but keep in mind that in complex cases, there may still be reasons to order the more complex outpatient labs on an inpatient, but generally they should only happen with specialist review and approval.
- The Order Sets
So now you’re faced with the question: one order set, or four order sets?
If you do one order set, you’ll probably end up needing to stratify them (with radio buttons!) into the four different workflows, e.g.:
Or, more likely for operational, culture, and other EMR configuration reasons, you may end up with four different order sets, in which case you will want to choose your naming convention very carefully, eg:
- Lumbar Puncture (LP) – Inpatient/ED at Bedside
- Lumbar Puncture (LP) – Inpatient/ED in IR
- Lumbar Puncture (LP) – Ambulatory/Outpatient in IR
- Lumbar Puncture (LP) – Ambulatory/Outpatient in Clinic
Even though #1 and #2 above are typically used by generalists, and #3 and #4 above are typically used by specialists. You’ll still want to have specialty input into #1 and #2, to help make sure that the common specialty scenarios can still be addressed (when they arise) in the inpatient settings. (For example, having Infectious Disease provide input into #1 and #2 can help make sure your ED providers/Hospitalists/Intensivists are ordering the right ID labs for the right scenarios.)
In my next post, we will look at these four LP workflows in more detail, and discuss some of the common educational, operational, and ordering challenges that organizations may come across when building out and optimizing these order sets.
This piece was written Dirk Stanley, MD, a board-certified hospitalist, informaticist, workflow designer, and CMIO, on his blog, CMIO Perspective. To follow him on Twitter, click here.




Share Your Thoughts
You must be logged in to post a comment.