The FDA has been receiving a great deal of criticism from the clinical community about a variety of issues, but probably none is as contentious as the ongoing patient safety issues regarding harmful drug-drug interactions and drug-gene interactions, estimated by the Institute of Medicine to cause 250,000 deaths each year in the U.S.
The current generation of physicians has generally not been well-educated in the application of post-genomic medicine to clinical practice. Many pharmacists do not have the training in basic science, such as advanced biochemistry, pharmacology and genetics to be proficient in this domain.
The differences in response to medications are always greater between members of a population than they are within the same person or between monozygotic twins at different times. The existence of large population differences with small intra-patient variability is consistent with inheritance as a determinant of drug response. It is estimated that genetics can account for 30 to 95% of variability in drug disposition and effects. Genetic polymorphisms in drug-metabolizing enzymes, transporters, receptors, and other drug targets have been linked to inter-individual differences in the efficacy and toxicity of many medications.
The FDA has prepared draft language that will become an annual certification requirement for most medical specialties. The FDA Certification Requirement in Pharmacogenetics will be phased in as of 2012 – 2015, with certain hospital-based medical specialties being the first to undergo Annual Certification. The curriculum needed to educate clinicians will be developed by independent organizations, following guidelines developed by the FDA.
The draft language contains the following learning objectives:
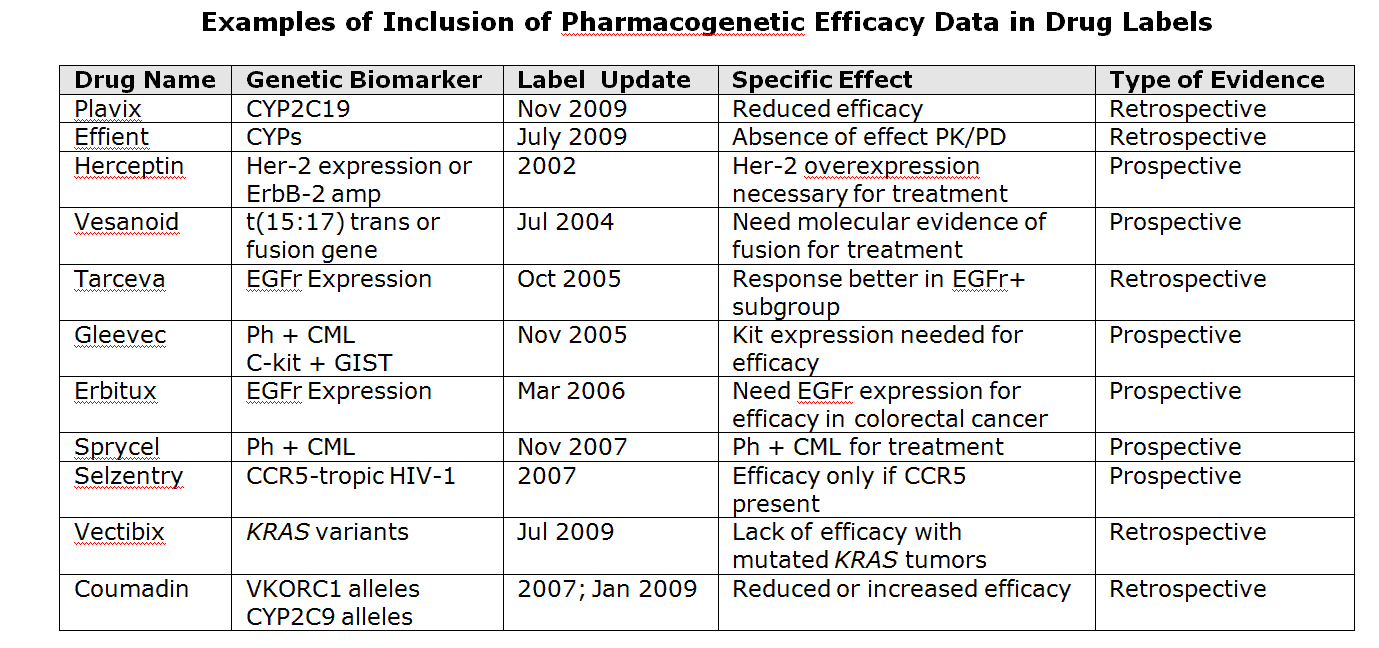
“Demonstrable knowledge of pharmacogenomic and related safety and efficacy pharmacologic knowledge contained in Drug Labels, including the following:
- When to perform a gene test or molecular diagnostic test based on the patient’s genetic composition.
- Interpretation and knowledge of risk alleles and other personal genomic data from gene test/molecular diagnostic results that determine use and dose.
- Understand pharmacokinetics and pharmacodynamics to the extent that determination can be made of possible harmful drug-drug and drug-gene allele interactions for individual patients.
- The ability to perform a comprehensive family history and interpret the results as they apply to pharmaceutical dosing.”
As previously suggested in a previous blog, the delivery of content and learning management may be based on the Electronic Health Record (EHR), or through other software applications.



Share Your Thoughts
You must be logged in to post a comment.